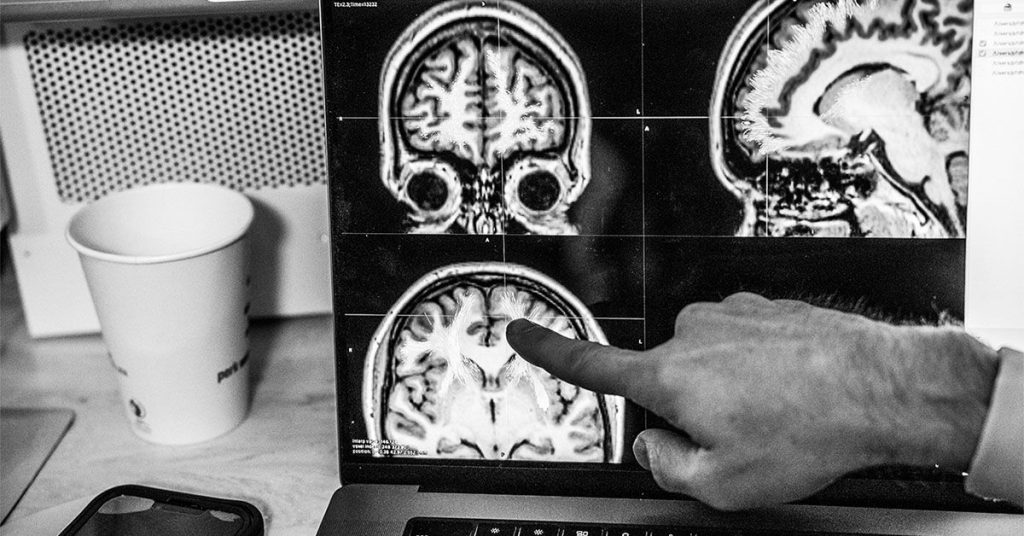
Recovery after a stroke can be unpredictable and influenced by many factors, including age-related brain changes. A recent observational study explored the potential link between age-related damage to parts of the brain containing white matter and stroke recovery. The study, published in Neurology, used MRI images to measure brain damage from a stroke, specifically focusing on white matter hyperintensities (WMH), which are sites of damage in the brain. Lead author Sook-Lei Liew, PhD, emphasized the importance of considering global brain health in stroke recovery and investigating other brain health markers to better understand motor control post-stroke.
Researchers utilized data from the ENIGMA Stroke Recovery Working Group, tracking 223 stroke patients across multiple research sites in various countries. Data collection occurred around 147 days post-stroke, with participants at different stages of recovery. The study found that both white matter hyperintensity size and the area affected by the stroke were positively associated with motor control symptoms. Those with fewer WMH showed a stronger correlation between motor control symptoms and the size of the area affected by the stroke, while individuals with larger WMH exhibited a greater correlation with cortical spinal tract damage. Interestingly, there were no significant differences observed between males and females in this study.
White matter hyperintensities are areas where fluid accumulates in the brain, often seen in individuals over 60 and associated with aging. These areas have been shown to increase with age and are linked to cognition and Alzheimer’s disease risk. White matter hyperintensity volume has been found to be correlated with shorter telomere length, which are structures at the end of chromosomes that shorten with age. Inflammation and ischemic injury are known mechanisms that can cause white matter disease and hyperintensities, impacting electrical signal conduction between neurons and potentially affecting neuroplasticity and compensatory neural network activity.
The researchers noted that lifestyle modifications to reduce high blood pressure can benefit in reducing white matter hyperintensities and associated risks. The next steps for the researchers involve identifying biomarkers of white matter hyperintensities, developing novel imaging sequences and serum assays to reliably detect markers of small vessel disease and abnormal blood-brain barrier opening that contribute to the appearance of WMH. By better understanding the relationship between age-related white matter changes and stroke recovery, there is potential for significant impact on preventing end-stage diseases such as stroke or dementia. Early secondary prevention strategies can play a crucial role in positively influencing individuals at risk for such diseases.