Researchers from Duke University recently conducted a study on diagnosing osteoarthritis in the knee and found biomarkers in the blood that can predict the development of the condition. The study showed that these biomarkers can predict osteoarthritis up to eight years earlier than the condition can be detected by X-ray, allowing for potentially earlier interventions to slow or halt the progression of the disease. This is significant as osteoarthritis is a common condition that affects almost all joints and currently has no cure. By identifying biomarkers for early detection, researchers hope to improve treatment outcomes for individuals with osteoarthritis.
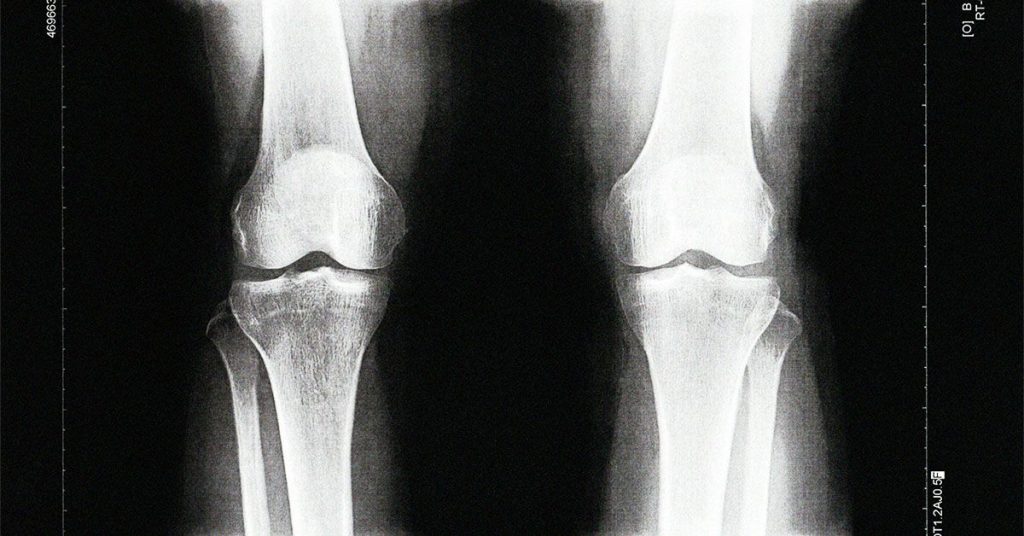
Osteoarthritis is the most common form of arthritis, affecting around 20% of adults in the U.S. It occurs when cartilage and other tissues in the joints begin to break down, leading to pain and limited movement. Risk factors for developing OA include joint injuries, age, obesity, and genetics. While the disease is irreversible, treatments such as weight loss, exercise, and medications like NSAIDs can help manage its progression. Early detection of osteoarthritis is crucial in preventing further damage to the joints, which is why researchers are focusing on identifying biomarkers that can predict the development of the disease well before it shows up on X-ray imaging.
The study by Duke University researchers focused on analyzing blood serum from a group of women to identify biomarkers that could serve as predictors for osteoarthritis in the knee. By examining serum samples from women who participated in the Chingford 1,000 Women study, the researchers were able to narrow down a set of biomarkers that consistently predicted the development of OA across all analyses. These biomarkers predicted OA development with a 77% accuracy, which was superior to predictions based on factors like BMI or knee pain. The genes linked to these biomarkers were found to be active in the cartilage and synovium of the knee joint, indicating their importance in understanding OA.
While the study results are promising, there are some weaknesses that need to be addressed. The study population consisted of a small cohort of white women, which may limit the generalizability of the findings to other populations at risk of developing osteoarthritis. Additionally, the study design as a case-control study may introduce biases that could affect the accuracy of the results. Despite these limitations, experts in the field believe that the development of a blood test for predicting knee osteoarthritis before structural damage appears on X-ray is a significant advancement in the field.
Experts emphasize the importance of early detection of osteoarthritis to help individuals at risk receive early interventions that can potentially slow or halt the progression of the disease. While the biomarker test identified in the study may not be available for public use immediately, it offers a promising avenue for improving the quality of life for individuals living with osteoarthritis. By controlling weight, maintaining or improving muscle strength, and engaging in healthy lifestyle habits, individuals at risk for developing OA can take steps to reduce the impact of the disease on their joints. Overall, the identification of sensitive biomarkers for early detection of osteoarthritis has the potential to reduce the medical burden of the disease and improve treatment outcomes for affected individuals.