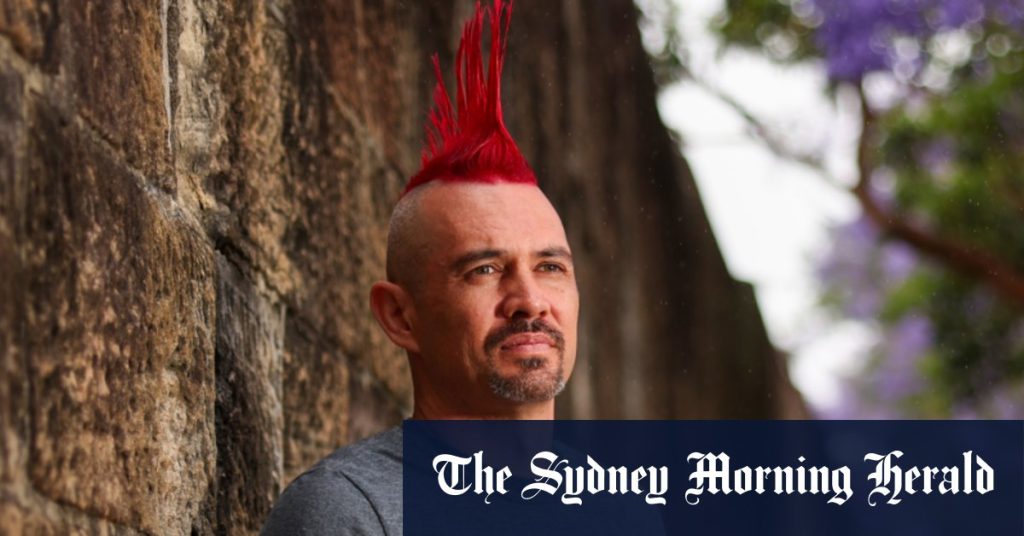
Summarize this content to 2000 words in 6 paragraphs Normal text sizeLarger text sizeVery large text sizeDamien Linnane will eat almost anything. Just don’t give him a green pear.In prison, he would eat five a day. Corrective services were obliged to provide at least one source of fruit, but they were so unripe that few people touched them – unless they needed a makeshift weapon.“There were actually assaults with these pears,” Linnane says, over lunch at Paddington’s Ampersand Cafe and Bookstore. “They were rock-hard.”We’re sitting just a few blocks from where Linnane was born at the old Royal Hospital for Women campus on Flinton Street. His parents met while his father was an inmate and his mother was a welfare officer at Long Bay jail, but the turbulent, at times violent, relationship ended before Linnane’s fourth birthday. He spent the rest of his childhood bouncing between a physically abusive father and a mother living below the poverty line.Damien Linnane explains his typical prison meal: a sausage roll for lunch, a microwave meal for dinner … and five pears for dessert. Credit: Dylan CokerThe years between then and his own incarceration are remarkable memoir fodder: he got caught up with a group of white supremacists as a teenager in Newcastle, handed out Sinn Fein flyers in Dublin, returned home to join the army reserves, worked part-time as a male prostitute for female clients in regional Armidale, and spent his 30th birthday serving a prison sentence for arson. “My partner told me she was raped, so I burnt down the house of the guy who did it,” is the short version of that story.Linnane has, by his own admission, come a long way since then. He taught himself to draw in prison, he has hung his art in exhibitions and he has published two books – his memoir and a fiction novel he wrote in prison on loose scraps of paper bound together with cable ties. He lives in a comfortable unit on a quiet street in Newcastle, splitting his time between editing a literary magazine for prisoners and researching a PhD on access to healthcare inside Australia’s jails. Late last year, he published his fourth academic paper in the Journal of Law and Medicine with no revisions.Before his arrest, Linnane was uncomfortable with attention. He wore combat boots, military fatigues and cut his hair short. “I was a paranoid person, and I was looking for ways to feel safer … if my hair is too short to grab in a fight, that’s a very, very slight advantage,” he says.That clearly isn’t an issue any more. It’s drizzling when we meet, and Linnane has brought a hairdryer in case the rain messes with his freshly dyed mohawk. He first grew it out during COVID lockdowns, and as his advocacy work grew, he found it was a handy conversation starter. “A part of it, I think, is compensating for being a bit of a paranoid wreck,” he says.If his journey sounds like the classic prison redemption arc, it’s only half the story. In truth (or at least Linnane’s version of it), he had started to turn a corner by the time the law caught up with him. “Before I was arrested, I realised I needed to talk to someone,” he says.Some of Linanne’s art from his time in prison.He booked in with a psychologist, who began to pick through a traumatic childhood marred by physical and sexual abuse, and the complications arising from his undiagnosed autism.Linnane was making progress. Then he was locked up. He assumed his therapy would continue inside, but a mandatory appointment with the prison psychologist quickly dashed those hopes. “She said, ‘Damien, everyone in prison would benefit from therapy, but there’s no funding for that’,” Linnane says.The psychologist’s job was to assess whether people were suicidal or dangerous. He was neither and so he was knocked back. A few days before Christmas 2015, he approached the guards at Glen Innes Correctional Centre and told them he was having suicidal thoughts. “They responded by putting me in solitary confinement,” he says.In a statement, a Corrective Services NSW spokesman said solitary confinement has been outlawed in NSW since 2014, but those assessed to be at risk of suicide or self-harm could be placed in a safe cell.“We take seriously our responsibility to reduce the possibility of [an] inmate harming themselves while in custody,” the spokesman said. “CSNSW does not comment on the management of individual inmates.”The setback proved formative. He wrote to then-prisons minister David Elliott, asking why he wasn’t able to see his psychologist in prison.The response, coming months later when Linnane had already been released, was a study in bizarre bureaucratic logic. The ministry had said prison resources were finite and therefore therapeutic programs were targeted “at inmates with the highest risk of reoffending”, but it then went on to argue that those inmates who fell outside this group couldn’t use Medicare-funded services because NSW prisons already provided mental health support.“That letter was the first time I realised I had lost my Medicare access,” Linnane says. “It was always in the back of my mind. Why has nobody tried to fix this?”It is a question that has consumed Linnane ever since. Now, he thinks he has the answer, and it flies in the face of half a century of legal precedent.Since 1973, it has been assumed that one section of the Health Insurance Act prevents Medicare benefits from being paid where that service is already provided by someone else (in Linnane’s case, the state government).But Linnane says he wasn’t offered anything in prison that compared with his Medicare-funded psychologist. Worse than that, he wasn’t given any treatment at all. He’s not alone. We’ve been talking about prison healthcare for almost three hours by the time our mains arrive, and his beef cheek pappardelle is getting cold as he reels off a long list of inmates who could have benefited from Medicare-funded healthcare.The beef cheek pappardelle at Ampersand Café and Bookstore in Paddington. Credit: Dylan CokerThere’s the devastating case of Douglas “Mootijah” Shillingsworth, a Budjiti and Murrawarri man who died in custody in Cessnock Correctional Centre after acquiring an ear infection that could have been picked up by a yearly Aboriginal health assessment usually bulk-billed but unavailable to those in custody.LoadingThen there’s the tragic death of Mulvan Jovanoski, who threw himself from a second-storey walkway at a Victorian prison after the state’s prison authorities failed to transfer him for cancer treatment on three separate occasions.In December, NSW deputy coroner Erin Kennedy recommended employing state-funded psychologists to provide therapeutic services to inmates following the death of Simon Cartwright, a 41-year-old with schizophrenia and bipolar disorder who had the water turned off to his prison cell as a punishment for his erratic behaviour.All of this was before the mass resignation of more than half of Justice Health psychiatrists working in the prison system. If mental healthcare was tough to get before, doctors and prison advocates warn it will now be almost impossible.Advocates and academics have campaigned for Medicare in prisons for decades, but those efforts have focused on lobbying governments to change legislation or relying on the federal health minister to grant exemptions in individual cases. But when Linnane organised a conference at the University of Newcastle’s Sydney campus last year, a third option emerged.After seeing her research in an investigation into Medicare fraud published in this masthead, Linnane asked Dr Margaret Faux to examine the laws governing Medicare in prisons.The billCredit: Dylan CokerIn her presentation, Faux said there was nothing in the Health Insurance Act that extinguished prisoners’ constitutional right to enter into contracts with private medical professionals. “Prisoners can – and do – enter contracts with private lawyers,” Faux told me. “Why can’t prisoners enter contracts with private doctors? It just didn’t make sense to me.”The theory captured Linnane’s attention, and the pair began drafting an academic paper that would flesh out their argument. They enlisted the help of Anthony Levin, a human rights lawyer at Legal Aid NSW, who reached the same conclusion: there is no legal case for denying prisoners Medicare in circumstances where no equivalent service is provided by the prison.They are now in the process of finding prisoners willing to test the law and they have psychologists, psychiatrists and nurse practitioners on standby to deliver bulk-billed appointments either through the audiovisual link system already used by lawyers, by phone appointments, or by enabling telehealth on prison-issued tablets.If a prison were to refuse, that would “likely be the trigger for a legal challenge”, Faux says. Loading“The beauty of this proposal is that this right already exists. No law needs to change,” Faux says. “We actually don’t need politicians to do anything. Isn’t that great? We just basically need them to get out of the way.”Other academics have studied prison healthcare but, as far as Linnane knows, he is the only one who has actually been to prison.That, Faux says, has enabled him to come up with a “totally novel” solution to a decades-long problem.“I would never have looked at this had it not been for Damien,” she says. “I’ve learnt a lot from Damien, and learnt how tough he is and has had to be, you know. He’s a real survivor.”Linnane is driven, but he is also a pragmatist. He sometimes worries his mohawk makes him look more punk than he actually is.“I’m a very realistic person,” he says. “Why am I working on Medicare? Because I honestly think I can make it happen.“Can I abolish prisons? No. Can I completely change the prison healthcare system? Also, probably not. But I think this is very achievable.”Start the day with a summary of the day’s most important and interesting stories, analysis and insights. Sign up for our Morning Edition newsletter.
Keep Reading
Subscribe to Updates
Get the latest creative news from FooBar about art, design and business.
© 2025 Globe Timeline. All Rights Reserved.