A comprehensive new analysis involving over 13,000 people has revealed that changes to blood vessels in the brain, which can increase the risk of stroke and dementia, are common in individuals with various heart conditions. The research, published in Neurology®, the medical journal of the American Academy of Neurology, is the most extensive systematic review of these ‘hidden’ brain changes to date. Lead author Dr. Zien Zhou from The George Institute for Global Health emphasized that identifying these changes could play a crucial role in determining appropriate treatments for these patients. People with heart disease are at a significantly higher risk of developing these brain vascular changes, even if they have not experienced a stroke, highlighting the importance of monitoring and addressing these issues in this population.
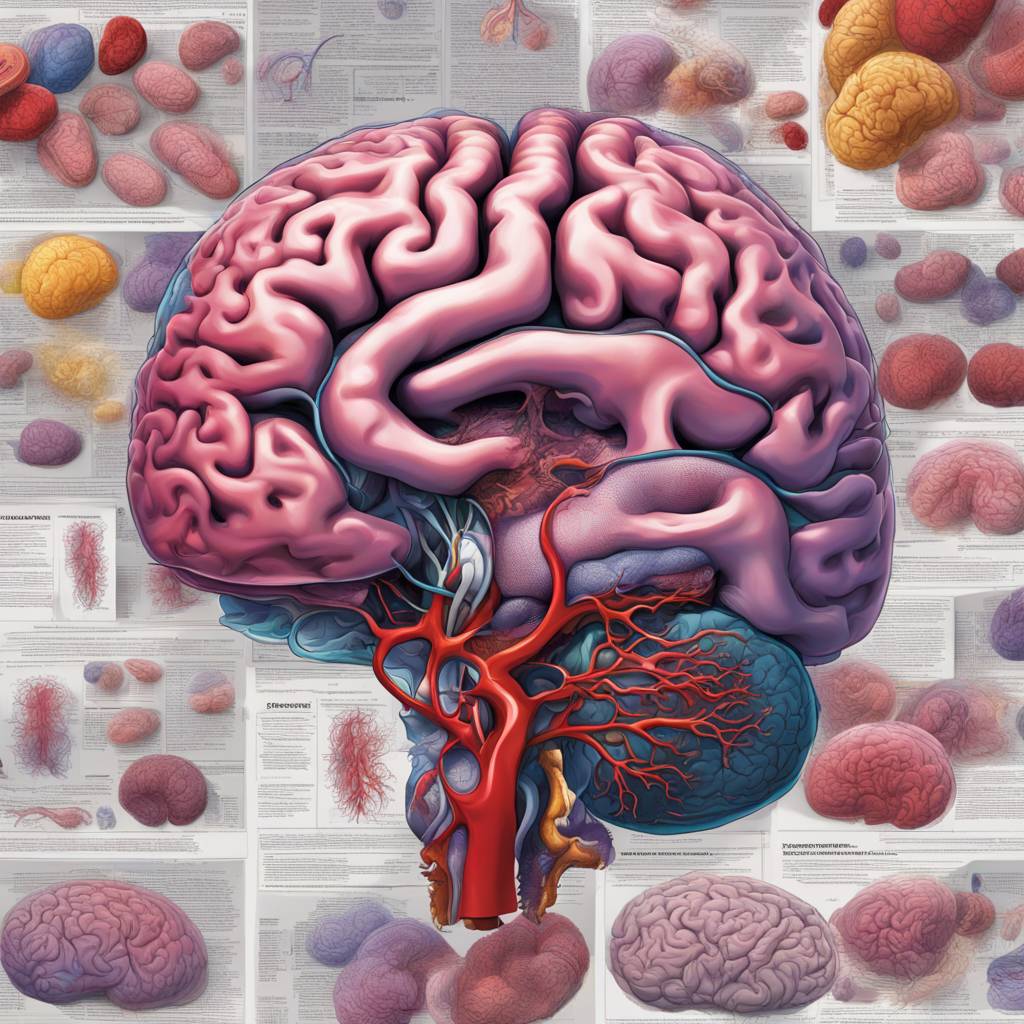
The study found that brain changes, such as silent brain infarction (SBI), lacune, white matter lesions, asymptomatic microbleeds, and brain atrophy, were prevalent in individuals with heart disease. These changes, which can only be detected through brain imaging, are known to occur more frequently in older individuals or those with hypertension. While they may not cause immediate neurological symptoms, they can lead to subtle deficits and increase the long-term risk of stroke or dementia. The research focused on adults with conditions such as atrial fibrillation, coronary artery disease, heart failure, heart valve disease, and patent foramen ovale, providing valuable insights into the prevalence of hidden cerebrovascular changes in these populations.
The findings revealed that approximately one-third of individuals with heart disease had some form of SBI, while a quarter exhibited lacune and two-thirds had white matter lesions. Additionally, a quarter of participants showed evidence of asymptomatic microbleeds in brain tissue, and over half had brain atrophy. Interestingly, the prevalence of these brain changes was similar between individuals with and without a recent stroke, with no apparent differences based on gender. Dr. Zhou highlighted that heart disease is a primary contributor to these brain changes, reflecting brain ‘frailty’ in individuals with these conditions.
The study indicated that common risk factors such as aging, hypertension, type 2 diabetes, hyperlipidemia, and smoking may contribute to the association between heart disease and hidden cerebrovascular injuries. The researchers suggested that a gradual decline in cardiac output in some patients with heart disease could impact blood flow to the brain tissue, leading to vascular changes and cognitive dysfunction. Furthermore, they proposed that hidden brain changes and cognitive issues could result from small blood clots traveling to the brain through arterial circulation after forming in the heart. Dr. Zhou emphasized the need for further research to explore the exact causes of these brain changes and their implications for managing individuals with heart disease.
More investigations are required to determine the precise mechanisms linking heart disease and hidden cerebrovascular injuries, as well as the potential approaches to managing these patients. The researchers emphasized the importance of understanding whether additional brain imaging, such as MRI, in individuals being considered for anticoagulation therapy is cost-effective in preventing adverse side effects. By refining the risks of brain clots and bleeds associated with anticoagulants and using this information to inform treatment decisions, the safety and efficacy of treatment for individuals with heart disease could be enhanced. The study underscores the significance of addressing these hidden brain changes in individuals with heart conditions to improve outcomes and quality of life for these patients.