New research conducted by scientists at the Max Planck Institute suggests that glial cells also play a crucial role in producing amyloid beta, a key protein linked to Alzheimer’s disease. This discovery challenges the long-held belief that neurons were the primary source of amyloid beta and opens up new possibilities for treatment approaches. Alzheimer’s disease, the most common form of dementia globally, currently has no cure, but therapies targeting amyloid plaques in the brain may help to slow disease progression at an early stage.
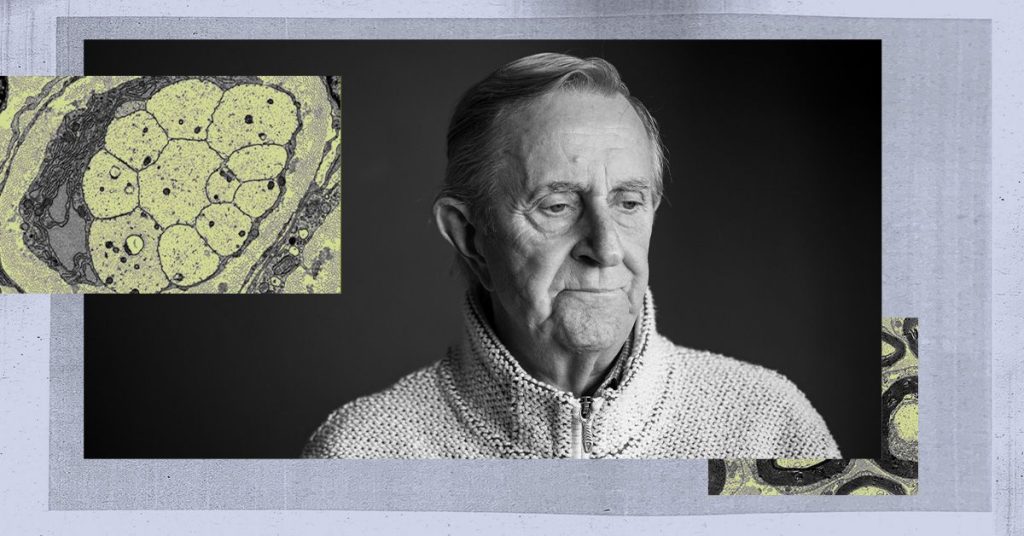
Beta-amyloid is a naturally occurring brain protein that accumulates in insoluble clusters, forming plaques between neurons and causing damage. The recent study from the Max Planck Institute reveals that in addition to neurons, certain glial cells in the brain also produce amyloid beta. By selectively disabling the enzyme BACE1 in neurons and oligodendrocytes of mice, researchers were able to observe how plaque formation across the entire brain was impacted. Removing BACE1 from neurons led to a significant decrease in plaques, while oligodendrocytes showed a 30 percent reduction in plaque formation.
The findings suggest that amyloid plaques only form when a specific level of amyloid beta from neurons is present, at which point oligodendrocytes contribute to plaque build-up. By inhibiting BACE1 effectively before this threshold is reached, researchers believe that plaque formation could be delayed, potentially slowing the early progression of Alzheimer’s disease. This new understanding of the role of glial cells in amyloid beta production may lead to the development of alternative treatment strategies aimed at targeting these cells alongside neurons.
The study’s first author, Andrew Octavian Sasmita, emphasizes that targeting oligodendroglial BACE and beta-amyloid production could serve as a viable approach for reducing amyloid beta levels in the brain. He suggests that anti-beta-amyloid therapies should be focused on very early stages of the disease before the threshold concentration of beta-amyloid is reached for plaque deposition. Sasmita also highlights the importance of considering the off-target effects of BACE inhibition, which have previously led to cognitive decline and brain shrinkage in clinical trials.
Bryen Jordan, a professor of neuroscience not involved in the study, commends the research for challenging the neuron-centric view of beta-amyloid production and shedding light on the significant contribution of oligodendrocytes. He believes that redirecting funding towards research involving glial cells could lead to new therapeutic developments that target both neurons and glial cells. The study’s findings also suggest that white matter abnormalities observed in Alzheimer’s patients may play a more primary role in the disease’s pathophysiology, potentially opening up new avenues for treatment.
In conclusion, by expanding the focus of Alzheimer’s research to include glial cells, this study may help overcome the limitations of previous therapies that solely targeted neurons. The recognition of oligodendrocytes as key contributors to beta-amyloid production may lead to the development of novel treatment approaches that could improve outcomes for individuals with Alzheimer’s disease. This new research highlights the importance of considering the complex interactions between different types of brain cells in the pathogenesis of neurodegenerative diseases like Alzheimer’s.