Newborn babies have one of three pioneer bacteria in their gut shortly after birth, one of which could be used to develop new personalised infant therapeutic probiotics. Researchers from the Wellcome Sanger Institute, University College London (UCL), and the University of Birmingham analysed stool samples from 1,288 healthy infants under one month old from the UK Baby Biome Study. They found that one of these beneficial bacterial pioneers was genetically adapted to make use of the nutrients in breast milk, suggesting it is best suited to thrive in a baby’s microbiome and can block pathogens from colonising the gut.
The findings from this study could support the development of infant formulas and therapeutic probiotics containing the most effective natural strains for the baby’s gut. The study revealed that most commercial infant probiotics contain a different bacterial strain not commonly found in infants in industrialised societies like the UK and the US. In addition to the two beneficial pioneer bacteria, researchers identified a third bacterium considered risky as it could lead to the colonisation of antibiotic-resistant bacteria, interfering with healthy microbiome development and increasing the risk of pathogen colonisation.
By mapping a baby’s gut microbiome profile right after birth to assess which pioneer bacteria they have, it may be possible to predict how their gut will develop. Personalised probiotics could then be provided if needed to promote healthy microbiome development and protect against potentially pathogenic infections. Further research is needed, such as the Microbes, Milk, Mental Health, and Me project, part of the Children Growing Up in Liverpool study, to understand the impact of pioneer bacteria on health, brain development, behavior, emotions, and mental health later in life.
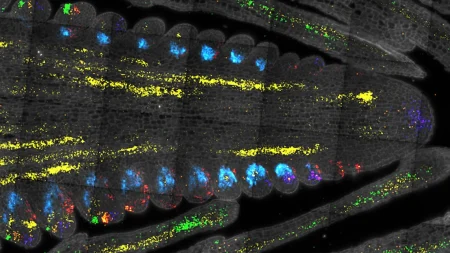
The gut microbiome is essential for human health and immune system development, beginning to form immediately at birth. The first month of life represents a critical window for intervention with probiotics to restore or boost the microbiome. The study analysed an expanded dataset of stool samples from 1,288 UK infants and identified three pioneer bacteria – Bifidobacterium longum subsp. longum, Bifidobacterium breve, and Enterococcus faecalis. B. longum and B. breve are beneficial, promoting the stable colonisation of other beneficial microbes, while E. faecalis is considered risky.
Researchers found that B. longum was passed from the mother’s gut during childbirth, while B. breve was not, suggesting another source of transmission, possibly the skin microbiome. The study also revealed that B. breve is genetically adapted to utilise the nutrients in breast milk and can block harmful pathogens from colonising the baby’s gut. While breastfeeding versus formula feeding did not seem to influence the type of pioneer bacteria, the use of antibiotics did. Other factors such as maternal age and birth count may also play a role, requiring further investigation.
The study highlights the potential for developing effective personalised interventions to support a healthy microbiome by understanding the make-up of the ecosystem and how it differs in infants. These interventions could include providing natural probiotics that fully digest breast milk and protect newborns against harmful microbes. The research aims to uncover how different pioneer bacteria affect health and diseases in childhood and later in life, with the UK Baby Biome Study actively following up participants for more insights. Larger cohorts are required to investigate the role of the infant microbiome on health and develop novel microbiome-based therapeutics based on genomic research.