Scientists from Duke-NUS Medical School and their collaborators have discovered an inherited genetic variation prevalent among East Asians that contributes to drug resistance in patients with chronic myeloid leukaemia. This variation drives aggressive cancer cell growth and reduces the effectiveness of conventional treatments. By inhibiting the action of a protein called MCL-1, the team has been able to effectively kill cancer cells resistant to standard treatments, offering promising results in laboratory studies. These findings, published in the journal Leukemia, highlight the importance of genetic profiling for developing precise and more effective cancer treatments.
Leukaemia accounts for a significant portion of new cancer cases and deaths globally, with chronic myeloid leukaemia being a subtype that affects the bone marrow. The team focused on understanding how an inherited genetic variation impacts patients with leukaemia, specifically targeting those with a variation in the BIM protein. This variation, found in approximately 12 to 15% of East Asians, leads to the production of alternative versions of the BIM protein, allowing cancer cells to evade cell death and proliferate more aggressively, contributing to disease progression.
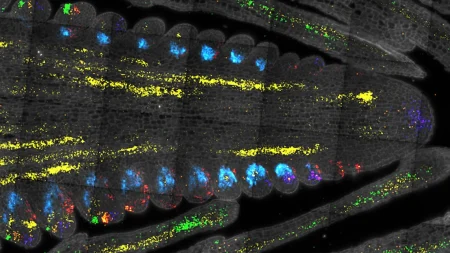
The researchers developed a pre-clinical model with the common genetic variation found among East Asians, enabling them to conduct experiments that demonstrated how the variation affects the survival and growth of cancer cells. Patients with this genetic variation often do not respond well to tyrosine kinase inhibitors like imatinib, a common treatment for chronic myeloid leukaemia. The resistance to imatinib observed in these patients is attributed to the higher survival rates and resistance to cell death induced by the treatment in cancer cells with the BIM variation.
Through advanced profiling techniques, the team identified that cancer cells with the BIM genetic variation rely heavily on the protein MCL-1 for survival. By targeting MCL-1, a potential vulnerability in imatinib-resistant cancer cells was revealed, opening up new possibilities for more effective treatments. Combining an MCL-1 blocker with imatinib showed promising results in killing resistant leukaemia cells, indicating that targeting MCL-1 could help address resistance in patients with the BIM genetic variation, potentially reducing disease progression and improving patient outcomes.
Collaborating with medical experts from Singapore General Hospital and National Cancer Centre Singapore, the researchers emphasized the importance of early and accurate cancer treatments to improve patient outcomes. Genetic testing for the BIM variation at diagnosis could help identify patients who may benefit from more aggressive treatments, offering a significant impact on cancer treatment outcomes. These findings could also extend to other types of cancer, such as certain lung cancers, where triggering the BIM protein is key to killing tumour cells, showcasing the potential for precision medicine to benefit a wider range of patients.
Duke-NUS Medical School is a global leader in medical education and biomedical research, focusing on translating basic scientific research into new treatment approaches for common diseases. By better understanding the genetic variations that affect cancer treatment outcomes, the team at Duke-NUS aims to deliver precision medicine to more patients, improving outcomes and quality of life. This groundbreaking research underscores the importance of genetic profiling in developing targeted and effective cancer treatments, offering hope for better outcomes for patients with resistant forms of leukaemia and potentially other types of cancer as well.