A study conducted by researchers at the UCLA Health Jonsson Comprehensive Cancer Center has shown promising results in treating non-small cell lung cancer by injecting engineered dendritic cells directly into cancerous lung tumors. By doing so, the researchers were able to boost the immune response and activate more T cells to attack the cancer more effectively. Combining this therapy with immune checkpoint blockade, a form of immunotherapy, further increased the treatment’s effectiveness in mouse models of non-small cell lung cancer.
Immune checkpoint blockade has been a game-changer in treating non-small cell lung cancer patients, but not all patients benefit from this treatment and some may experience disease progression after an initial positive response. This may happen due to the immune system failing to recognize the tumor as a threat or the tumor microenvironment suppressing the immune response. Chemokines, such as CXCL9 and CXCL10, have been identified as key molecules in attracting immune cells, particularly activated T cells, to the tumor site and enhancing the immune system’s ability to fight cancer effectively.
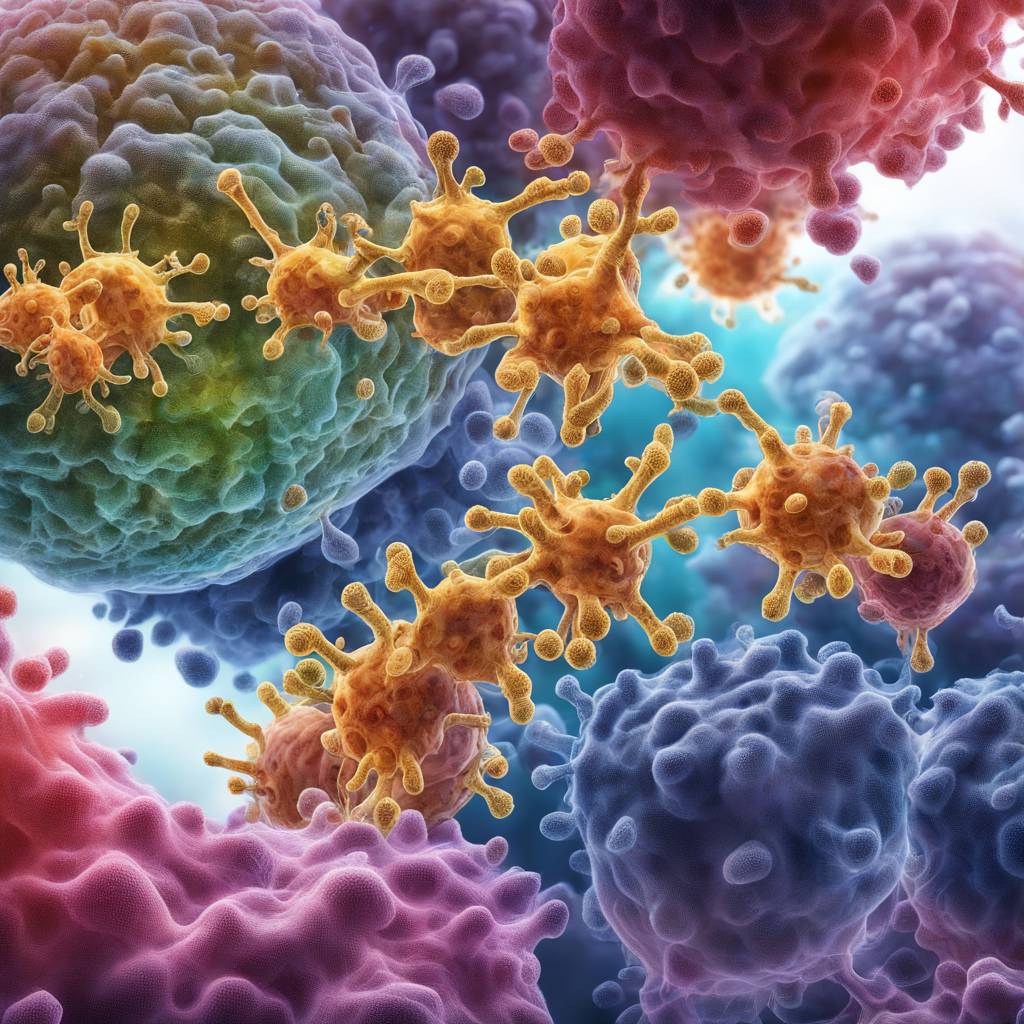
To improve the efficacy of immune checkpoint blockade, the UCLA team explored in situ vaccination with gene-modified dendritic cells, a method involving the direct injection of immune-stimulating, chemokine gene-engineered dendritic cells into the tumor. By genetically modifying dendritic cells to produce CXCL9 and CXCL10, the researchers aimed to increase T cell infiltration and activation within the tumor. This approach was successful in increasing the number and activity of T cells in the tumor, slowing down tumor growth in mouse models of non-small cell lung cancer, even in cases of tumor resistance to standard immunotherapy.
The findings from the UCLA study suggest that utilizing CXCL9 and CXCL10-producing dendritic cells in conjunction with immunotherapy could be a promising strategy to overcome treatment resistance and enhance clinical outcomes for non-small cell lung cancer patients. The therapy also showed potential in establishing a long-lasting immune response against the cancer, indicating its ability to provide sustained benefits to patients. Furthermore, genetic data analysis from lung cancer patients indicates that CXCL9/10-DC therapy could be particularly beneficial for individuals with specific genetic characteristics linked to resistance to standard immunotherapy.
In conclusion, the research conducted by the UCLA Health Jonsson Comprehensive Cancer Center highlights the potential of using engineered dendritic cells producing CXCL9 and CXCL10 alongside immune checkpoint blockade to enhance the immune response against non-small cell lung cancer. By targeting the tumor microenvironment and promoting T cell activation, this approach has shown promising results in preclinical studies and may offer a new treatment option for patients who have not responded well to standard immunotherapy. Further studies and clinical trials are needed to validate these findings and determine the therapy’s efficacy and safety in human patients.