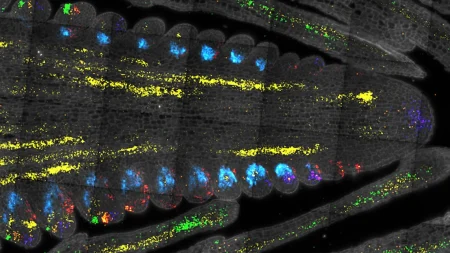
Glioblastoma is a highly aggressive primary brain tumor with a low survival rate and limited treatment options. In recent years, immunotherapies have shown promise in providing renewed hope for patients, although with only modest success. A team from the University of Geneva and the Geneva University Hospitals has identified a specific marker on the surface of tumor cells and generated immune cells, known as CAR-T cells, carrying an antibody to target and destroy these cells. These CAR-T cells have shown the ability to target diseased cells in the tumor that do not carry the antigen, while sparing healthy cells.
Denis Migliorini, an assistant professor and expert in CAR-T cells, has been working to identify protein markers expressed by glioblastoma cells. One of these markers, PTPRZ1, has been found to be particularly important, and CAR-T cells carrying antibodies targeting PTPRZ1 have shown promising results in targeting malignant gliomas. By introducing messenger RNA encoding for the desired antibody into T-cells, the researchers have created a flexible platform that allows for multiple adaptations based on the specificities and evolution of the tumor.
In vitro tests have shown that CAR-T cells effectively target and destroy tumor cells while sparing healthy cells. Additionally, these CAR-T cells have demonstrated a bystander effect, where they can identify and fight tumor cells that do not express the PTPRZ1 marker. In mouse models of human glioblastoma, CAR-T cells administered intratumorally have controlled tumor growth, significantly prolonging the lives of the mice without signs of toxicity. This data, along with other promising results, has led the researchers to consider moving towards a first clinical trial in humans.
The use of CAR-T cells offers a promising approach to treating glioblastoma, a difficult-to-treat type of brain tumor that often recurs rapidly. By genetically modifying immune T cells to express antibodies that target specific tumor cells, researchers are able to create a therapeutic approach that shows potential for improved efficacy and safety. The flexibility of the CAR-T cell platform allows for adaptations based on the tumor’s unique characteristics, making it a promising option for personalized treatment strategies.
The development of CAR-T cells using messenger RNA encoding for the desired antibody offers advantages over traditional viral vector techniques, particularly in the context of brain tumors. This approach reduces the risk of toxicity associated with long-term persistence of viral vectors and allows for the production of the receptor that recognizes the tumor target. By demonstrating efficacy and safety in preclinical studies, the team from the University of Geneva and the Geneva University Hospitals is paving the way for potential clinical trials with human patients, offering new hope for those diagnosed with glioblastoma.